Blood flow restriction (BFR) therapy is a therapeutic and fitness modality that involves semi-occluding (40%-80%) blood flow to the targeted limb with a pneumatic cuff(blood pressure cuff), while performing low intensity exercises. Yes, despite how it sounds, it is safe. This methodology, which was pioneered in 1966 by Dr. Yoshiaki Sato in Japan, reduces blood flow to the muscle, thereby turning on physiologic pathways that promote muscle growth and aerobic capacity at much lower exercise intensities than would otherwise be required. BFR therapy has gained significant attention in recent years due to its potential to enhance muscle strength, expedite post-injury recovery, and improve athletic performance.
BFR therapy provides muscle growth, both in size and strength, that is similar to that of high intensity exercise. When performing a low-load, high repetition exercise, we have a bias towards using our slow-twitch, endurance muscles fibers. These fibers are mitochondrial dense, requiring blood flow to produce energy. If that blood flow is reduced, as with BFR therapy, our body has no choice but to use the more powerful, fast twitch muscle fibers. These muscle fibers function in a low-blood flow environment because they store their energy locally, albeit in limited amounts. Consequently, you see the benefits of high-load training at less intense efforts.
Because of its ability to grow muscle and improve aerobic capacity at low intensities, BFR therapy has important implications in the rehabilitation setting. Athletes and non-athletic populations suffer from deficits in muscular coordination, strength and cardiovascular fitness when recovering from an injury. BFR therapy can strengthen neuromuscular pathways, improve muscle growth and strength as well as benefit the cardiovascular system. Thus, BFR therapy is an important tool throughout the rehabilitation timeline, from immediately post-surgical or post injury, to returning to your sport or fitness activity of choice.
When we have surgery or hurt a joint and/or any of the support tissue around a joint, the adjacent musculature begins to atrophy, often dramatically so. Additionally, the body often temporarily, “turns-off,” the neurological pathways around injuries that makes muscle contractions possible. BFR therapy has shown promise in improving the ability to strengthen the contraction of a muscle when the limb has been immobilized and/or there is diminished contraction strength to the musculature around the injury. In this context, blood flow is semi-occluded proximal to the injured joint while performing isometric contractions (muscular contractions without limb movement) are performed. As the neuromuscular pathway is strengthened, muscle coordination is improved resulting in increased muscle strength and adjacent joint stability.
Once a joint can be mobilized, BFR therapy is used to promote muscle strength and growth. Again, blood flow to the limb is semi-occluded and then the joint is actively moved throughout available range of motion. Initially, this is done without any resistance and with appropriate repetitions. As the muscle gets stronger and the range of motion improves, progressive amounts of weight can be used to further enhance muscle strength.
This therapy is not limited to acute injuries or post-surgical rehabilitation. BFR therapy can be applied to more chronic conditions that require joint movement for recovery. Moving an arthritic joint, especially under higher loads, can make walking, running, grasping and lifting difficult and painful. BFR therapy allows arthritis suffers the ability to build strength around joints without putting excessive stress on it.
While benefits in muscle growth in strength and size is mediated at the muscle fibers, blood flow restriction therapy elicits cardiovascular benefit as well. When this modality is applied during cardiovascular exercise, it limits return of blood through the venous system. This prompts the body to increase your heart rate, thus providing a faster heart rate at a lower cardiovascular intensity. In studies, the subjects aerobic capacity improved at a low load of 40% their VO2 max. With normal cardiovascular exercise, the subjects had to achieve 50% of their VO2 max to improve their aerobic capacity.
One of the most important components of returning patients to activity or sports is improvement and maintenance of their aerobic fitness. The postoperative period can negatively impact aerobic capacity in hospitalized or elderly individuals. Maintaining and improving aerobic capacity can be the crux of their functional recovery. Applying BFR therapy earlier in the rehabilitation cycle has important implications in time to return to sport, but can also provide important wellness benefits for the non-athletic and sedentary populations.
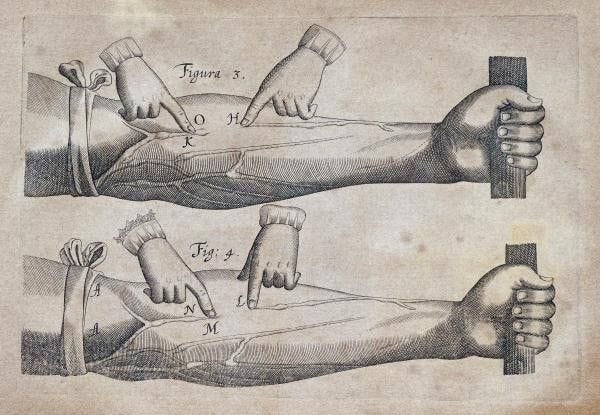
While a simple tourniquet can occlude blood flow, it is important and a much safer alternative to use specialized pneumatic cuffs. The cuffs I use are placed around the limb, then automatically inflate to take your blood pressure. The device then automatically calibrates the appropriate pressure to use based on your blood pressure. Alternatively the cuffs can be manually adjusted for comfort. Once inflated to the appropriate pressure, the patient will begin a series of high-repetition, low weight exercises on the targeted limb. The therapy should be repeated 2-3 times a week for 6-9 weeks or terminated when the patient can begin to perform higher intensity exercises without pain.
BFR therapy has emerged as a valuable tool for rehabilitation because of its role in muscle hypertrophy, and enhancement of aerobic capacity. Its ability to stimulate muscle growth and strength gains with lower loads makes it an accessible and effective rehabilitation modality for acute, post-surgical and chronic injuries. However, it is essential to note that proper training protocols, qualified supervision and appropriate equipment are necessary for the safe and effective implementation of BFR therapy.